Gas-sensing capsule takes another big step from lab to commercialisation
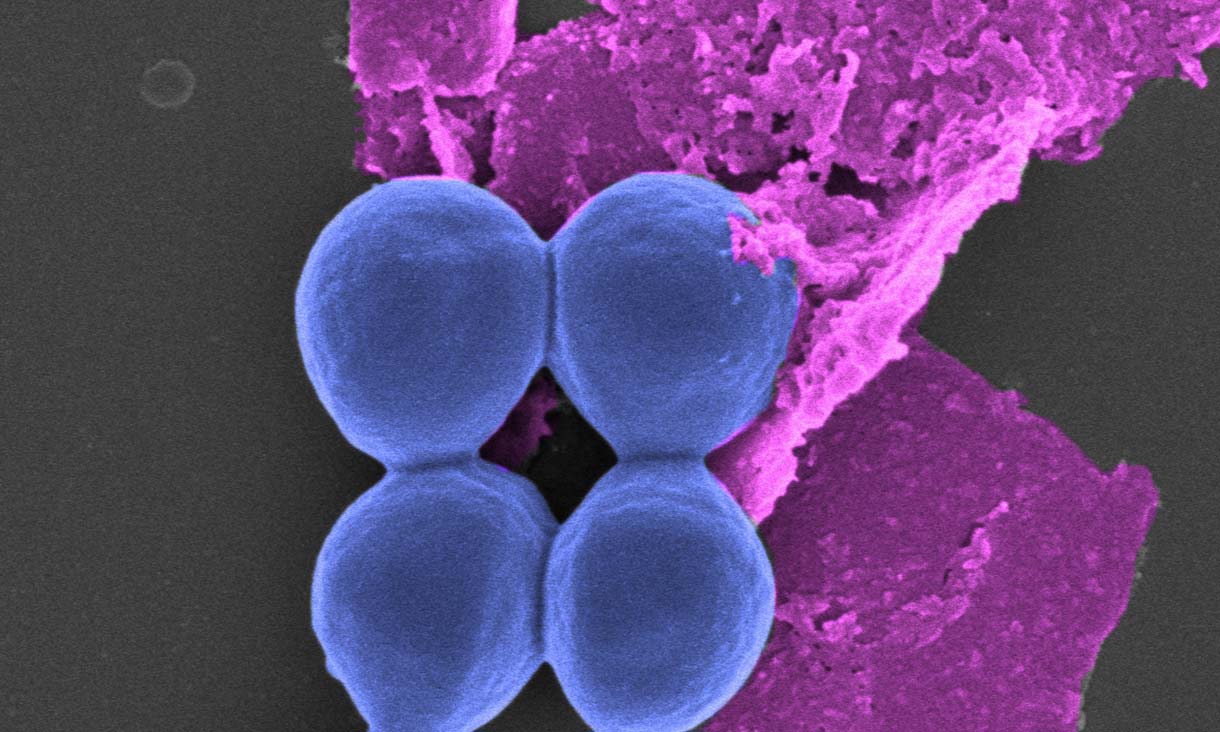
An ingestible gas-sensing capsule that provides real-time insights into gut health has moved closer to market with RMIT University transferring IP ownership to medical device company Atmo Biosciences.
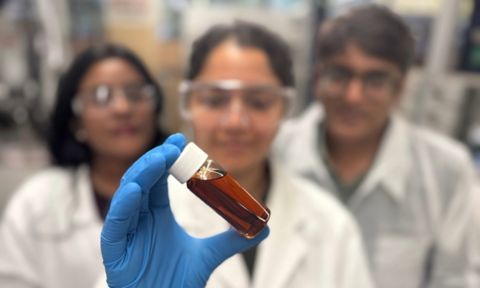
Aussie tech helps make bio-oils for greener industrial applications
Australian technology developed at RMIT University could enable more sustainable and cheaper production of bio-oils to replace petroleum-based products in electronic, construction and automotive applications.
RMIT Centre for Applied Quantum Technologies launches during International Year of Quantum
This week, RMIT Centre for Applied Quantum Technologies (RAQT) was launched by the University.