

Metastatic cancers – like lung, ovarian and breast cancer – break away from where they first form and create new tumours in other parts of the body. For example, people with lung cancer may have the tumour spreading into their bones.
Understanding where a cancer originates from is a key challenge for clinicians. One clue is in the ‘markers’ of cancer cells that detach from the tumour and circulate in the blood of cancer patients. These cells are particularly rare and can be one in a million, making them extremely difficult to find, let alone isolate.
Without the ability to efficiently identify where the cancer began and where it will spread, clinicians cannot prescribe the best treatment. For example, if the cancer began in the lungs and has already spread to the bones, treatment focused on the lung tumour alone would not be enough.
The interdisciplinary team of biomedical experts and technologists at the Integrated Photonics and Applications Centre are working backwards to find out more about the way cancer cells spread. They use already isolated samples of cancer cells to learn about their behaviour, and the signals they send to other cells once they’ve spread.
A key part to understanding circulating cancer cells is watching what they secrete. Messages in the secretions are sent to other cells, telling them to replicate and spread. Encoded in these messages are ways to protect themselves against drugs that will kill them. If we can identify them, then we will have more information to pinpoint these hidden codes to stop cancer spreading in the first place.
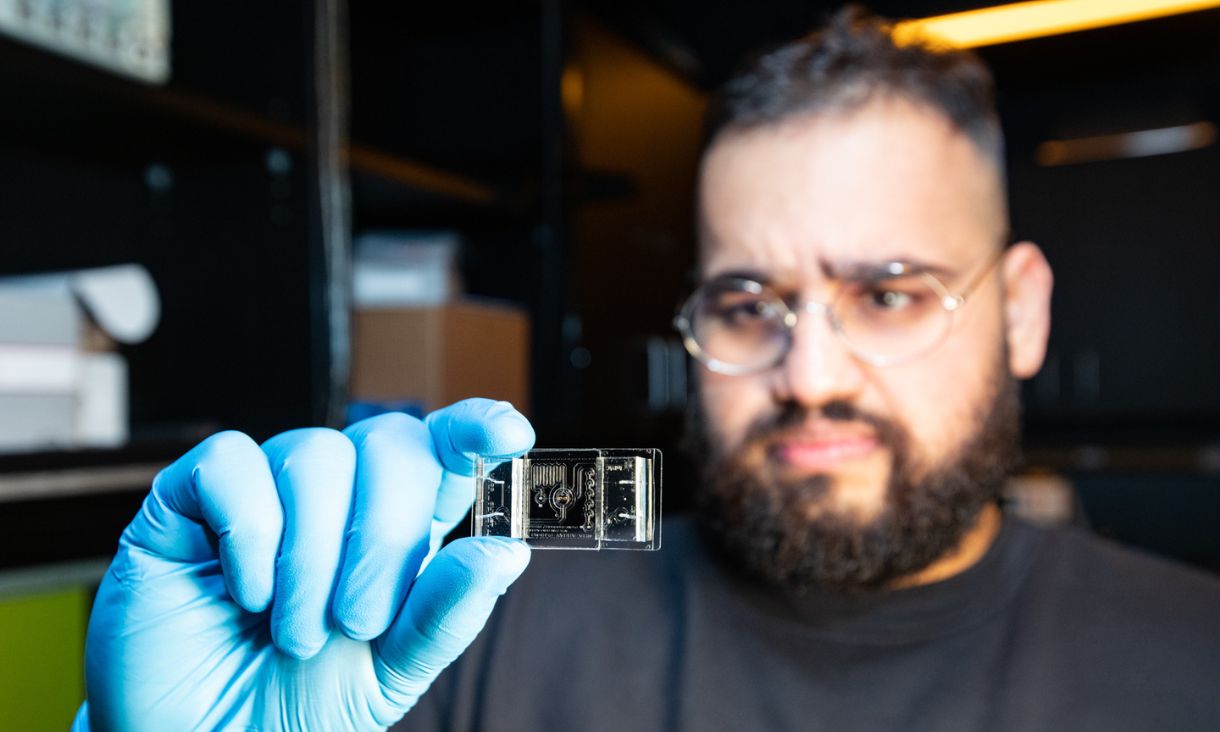
The team is using a technology called microfluidics – a tool with tiny channels that can filter out specific molecules like DNA or even specific cancer cells (see right). This mini-plumbing tool can isolate these cells and their secretion messages which can later be used as markers to look out for in patients.
This approach, paired with a light-powered photonics platform, miniaturises the sensor needed to detect and capture these cancer secretions. The result is a tiny sensor about 20 times smaller than a five-cent piece (see image right). The combination of these two technologies is extremely accurate at finding the circulating cancer tumour cells in very small samples.
These two approaches give the team a high level of control. They can capture and observe cancer cells to induce the secretion (or conversation). They can even introduce drugs to see how the cells respond.
By having such a controlled environment, the team can test:
how the cancer cells respond
the pattern of behaviour of different cells – whether it be how a breast cancer cell behaves compared to a lung cancer cell
which treatments respond best to different cancers.
This technology has many potential applications for any single cell and multi cell study – particularly for aiding chemotherapy treatments, discovering new drugs, or isolating immuno-compromised cells to manipulate them then re-introduce them back into the body.


PhD Cotutelle student at Ecole Centrale Lyon and RMIT University
Biomedical Team Leader, Integrated Photonics and Applications Centre
Postdoctoral Fellow, Integrated Photonics and Applications Centre
Director, Integrated Photonics and Applications Centre
Chemistry and Nanobiology Team, Ecole Centrale Lyon
Microfluidics Researcher, Institut des Nanotechnologies de Lyon, Univ. Lyon1, Ecole Centrale Lyon
Read the review article in Biosensors and Bioelectronics to find out more about our research.
This project, including the PhD position of Syed Harris Hussain, was made possible by ECLAUSion, a cotutelle PhD program between Ecole Centrale Lyon and RMIT University.


RMIT University acknowledges the people of the Woi wurrung and Boon wurrung language groups of the eastern Kulin Nation on whose unceded lands we conduct the business of the University. RMIT University respectfully acknowledges their Ancestors and Elders, past and present. RMIT also acknowledges the Traditional Custodians and their Ancestors of the lands and waters across Australia where we conduct our business - Artwork 'Sentient' by Hollie Johnson, Gunaikurnai and Monero Ngarigo.
More information